Natural Hazards
Pandemics
Prepared by CEMEC – European Center for Disaster Medicine Center – San Marino & the Editorial Board
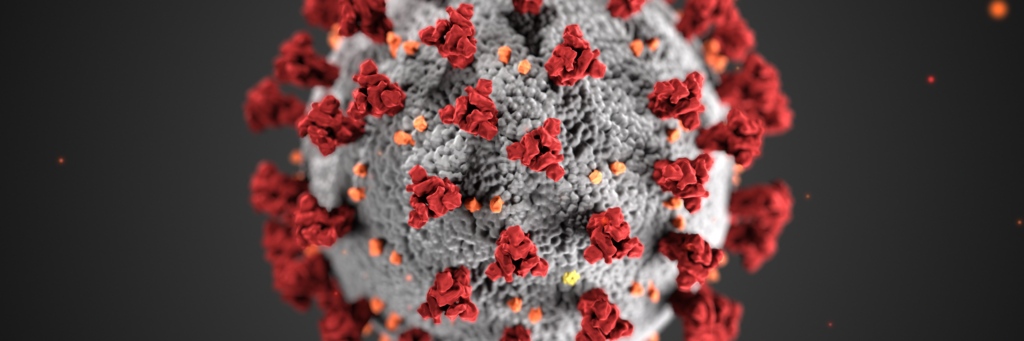
Biological hazard is a term applied to the possibility that biological agents cause disease, including pathogenic micro-organisms, viruses, toxins spores, fungi and vectors or transmitters of disease such as humans themselves, animals and plants.
These sources can cause various negative health effects ranging from skin irritation and allergies to infections and life-threatening diseases. Currently we are facing one of the most important health issues that the world has ever experienced with the ongoing so-called “novel coronavirus disease” or COVID-19 pandemics. Public health experts believe that mankind is at a greater risk than ever of experiencing large-scale outbreaks and global pandemics. Epidemics seem to spread faster and further than ever, outbreaks that were previously localized can now become pandemic very rapidly due to a series of factors such as population growth and globalization, and climate change. The direct health impacts of pandemics can be catastrophic, in terms of public health but also of economic and social wellbeing and have a significant psychological impact. Pandemic prevention plans need to be implemented worldwide.
Disease surveillance remains one of the highest-stakes areas of science; preventing pandemics by investing in research and analysing circumstances underlying outbreaks can save thousands of lives.

Recent pandemic events.
In this paper a few examples of pandemics are given. The history of pandemics shows that in the past, they were prevalently sustained by bacteria (e.g. plague, cholera, etc.), whereas since the 20th century, the main pandemics have been sustained by viruses, especially flu viruses.
The fears of the world health authorities are mainly about flu viruses, since new pandemics appear regularly at intervals of 20-40 years, correlated to the continual antigenic mixes of animal (swine, avian) and human flu viruses. This continual genetic recombination can also produce strains that are highly aggressive in humans, featuring rapid inter-human transmission due to the fertile terrain of an immune system that is inactive against the new virus since it has never before encountered that particular strain. The BeSafeNet website will help to better understand the occurrence, characteristics and impact of biological hazards; a theme that needs to be addressed by the schools.
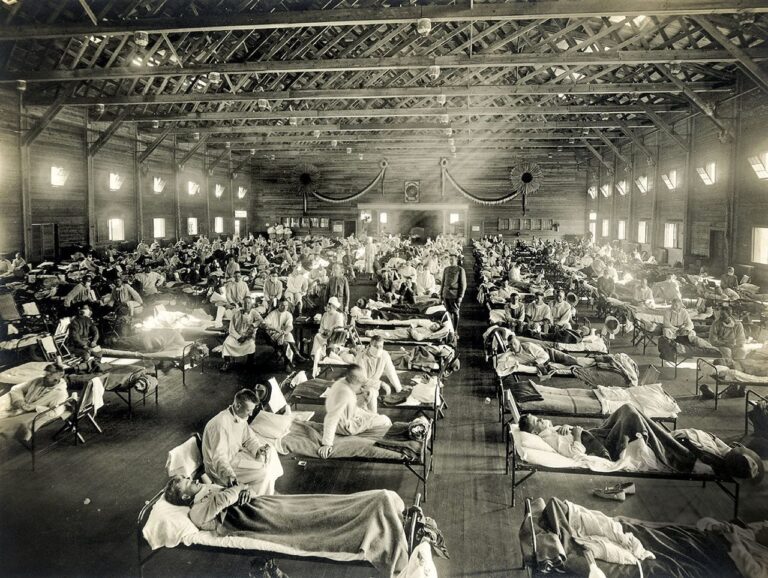
Spanish Flu 1918
During the 20th century, the Spanish flu affected one third of the world population and was particularly severe, causing an estimated number of deaths of between 50 and 100 million people, with social and economic consequences that lasted for the subsequent generations.
SARS 2002-2003
SARS (the acronym for Severe Acute Respiratory Syndrome) is an atypical form of pneumonia caused by a coronavirus that was responsible for an epidemic outbreak in the Far East between 2002 and 2003, that caused several hundred deaths. Thanks to the isolation of the virus, a vaccine was soon developed and efficacious treatments that contained the spread of the disease. The Italian physician who discovered it, Carlo Urbani, has gone down in the history of medicine as the man who first identified the disease, and lost his life to it.
Ebola 2014
In 2014, Ebola hit three African countries (Guinea, Liberia and Sierra Leone) and six other countries on three continents, causing alarm around the world.

Zika 2015
In 2015, the Zika virus, transmitted by the Aedes Aegypti mosquito, triggered a wave of microcephaly in Brazil, causing terrible damage to the brain during the embryonic stage, affecting more than 70 countries around the world.

Flu
Apart from historical examples, the most evident “modern” pandemic is the flu, that occurs with a more or less annual periodicity, in areas over several continents, almost simultaneously. Other examples of current pandemics are HIV/ AIDS (since 1981) and COVID-19 since 2019.
SARS-CoV2 2019
On 11 March 2020, the World Health Organization (WHO) declared a pandemic due to the new coronavirus 2019-nCoV, later called SARS-CoV2, that causes COVID-19 (Co: coronavirus Vi: virus, D: disease 19), isolated in man for the first time at the end of 2019 in Wuhan, China. Li Wenliang, the doctor in Wuhan who first spread the alarm about a new coronavirus, did not gain a sufficient hearing and was then accused by the Chinese police of spreading fake news. He contracted COVID-19 one month later and died at the age of only 34 years.
At present (towards the end of 2020) there have been about 29.5 million people infected in the world with almost 900,000 deaths. In descending order, the countries with the highest number of victims are the United States, Brazil, the United Kingdom and then Italy that was the first European country to face the virus. COVID-19 disease is often self-limiting and involves only flu-like symptoms, but it can be fatal because it can lead to pneumonia with acute respiratory syndrome and disseminated vasculitis in subjects with previous disease, immunosuppressed and the elderly. The course of the disease in children is self-limiting and resembles a common cold. There is currently no therapy that proves effective in COVID-19 disease; the therapy is mainly supportive based on antiviral drugs, for example antiretroviral drugs used in the treatment of HIV/AIDS, chloroquine or immunomodulatory drugs. Vaccine prophylaxis seems to be the most promising strategy to be able to defeat the Coronavirus, for which there is still no effective therapy.
One of the most important health issues faced by the world today is the threat of a global disease outbreak called a pandemic. A pandemic is an epidemic infectious disease that spreads rapidly to several areas of the world, affecting a very high number of people. In accordance with the WHO (World Health Organization) definition, a pandemic is declared if a new disease spreads worldwide involving at least two continents. When it is used in reference to contagious diseases or conditions, the risk is that the entire world population is likely to be exposed to the pathogenic agent and develop the disease. These diseases are caused by newly detected or re-emerging biological agents. Analysing the history of outbreaks caused by these agents and trends in epidemiological data can help to better identify the related risks for the whole population, and save lives.
Not all infectious disease-related terms have the same meaning, though often they’re mistakenly used interchangeably. The distinction between the words “pandemic,” “epidemic,” and “endemic” is regularly mistaken.
An epidemic is a disease that affects a large number of people within a community, population or region. A pandemic is an epidemic that spreads over multiple countries or continents. An outbreak is a greater-than-anticipated increase in the number of endemic cases. It can also be a single case in a new area. If it’s not quickly controlled, an outbreak can become an epidemic.
Endemic is a disease that is constantly present in a region for example malaria is endemic to parts of Africa.
What’s the difference between epidemic and endemic?
An epidemic is often localized to a region, but the number of those infected in that region is significantly higher than normal. For example, when COVID 19 was limited to Wuhan, China, it was an epidemic. The geographical spread turned it into a pandemic.
A pandemic is a global disease outbreak. It differs from an outbreak or epidemic because it:
- affects a wider geographical area, often worldwide.
- infects a greater number of people than an epidemic.
- is often caused by a new virus or a strain of virus that has not circulated among people for a long time. Humans usually have little to no immunity against it. The virus spreads quickly from person-to-person worldwide.
- it causes much higher numbers of deaths than epidemics.
it often creates social disruption, economic loss, and general hardship.
During an outbreak of human infectious disease, the numbers affected will vary depending on the disease, location, susceptible population size and the environment; the worst risk is that the infection can spread universally and become a pandemic. Biological agents can be transmitted through ingestion (accidental swallowing or via hand-to mouth contact), inhalation, sexual intercourse, through the membranes of the eyes, or through contact with broken skin. Thus, for the disease to develop, there needs to be sufficient numbers of the pathogenic micro-organisms to overcome the body’s defenses. This number differs from pathogen to pathogen and infectious doses for some pathogens are unknown, being further complicated by variation in susceptibility due to environmental/human metabolic factors.
In the 21st century, epidemics seem to spread faster and further than before. Outbreaks that were previously localized can now become pandemic very rapidly due to a series of factors: population growth, increasing urbanization, greater demand for animal protein, greater travel and connectivity between population centers, habitat loss, climate change etc. With the global population estimated to reach 9.7 billion by 2050 and with travel and trade steadily increasing, public health systems will have less time to detect and contain a pandemic before it spreads.
Public health experts believe that we are now at greater risk of experiencing large-scale outbreaks and global pandemics.
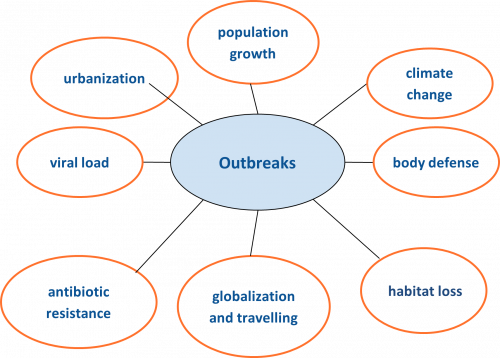
Globalization: fast and intense mobility of people, with increased transport and international travel, leads to rapid spread of infections. Thus, an individual flying from one side of the world can introduce a new disease into the other side within hours, and before even showing symptoms.
Population growth: as the population increases, so does the need for land and housing. Populations expand into previously uninhabited territories, such as forests. With new territories comes contact with new animals and, inevitably, new infections. In many affected countries, the weakness of the existing health care system prevents effective access to medical interventions, prevention of infections and control practices. Migration is also responsible for the increased risk of infections. Millions of people involved in many humanitarian emergencies, fleeing from civil unrest, political instability, conflicts, wars and natural disasters, have been uprooted from their homes and become refugees, asylum-seekers or economic migrants, and find themselves living in conditions that are often overcrowded, thereby becoming particularly vulnerable to illnesses. The conflicts and wars referred to above do not only cause civilian casualties and displacements; they destroy health care facilities exactly when and where they are most needed.

In the last decades, new infectious diseases have been recognized and some well-known diseases have appeared again. The combination of antibiotic misuse in human and veterinary medicine, antibiotic resistance as well as genetic mutation of bio-agents has caused a further rapidly emerging problem concerning the worldwide spread of infections. Viruses are infectious agents that are more likely to generate pandemics, as they are more able to adapt and to jump from one species to another.
Potentially hazardous changes are also taking place in the use of land, agricultural practices and food production, such as live poultry and animal markets and deforestation, with an increased demand for meat for human consumption – which also leads to increased contact between people and wildlife and the transmission of zoonoses (a sleeping sickness, which is caused by T brucei rhodesiense (or other) parasites which can be transmitted from animals to humans).

Evidence continues to emerge that climate change is resulting in greater numbers of heatwaves and flooding events, bringing more opportunity for waterborne diseases such as cholera and for disease vectors such as mosquitoes in new regions.

Infectious diseases do not respect boundaries, and a pandemic is by definition an epidemic infectious disease that spreads rapidly to several areas of the world, although evidence shows that new outbreaks usually start in Asia or Africa. Most new pandemics have originated through the “zoonotic” transmission of pathogens from animals to humans. Zoonoses from domesticated animals are concentrated in areas with intensive and extensive farming and livestock production systems and live animal markets.
Dense concentrations of population, especially in urban centers, can act as focal points for disease transmission and accelerate the spread of pathogens. Moreover, social inequality, poverty, malnutrition, and calorie deficits weaken an individual’s immune system, while environmental factors such as lack of clean water and adequate sanitation amplify transmission rates and increase morbidity and mortality. An unprecedented shift in human population with rapid urbanization is one reason why more diseases originate in Asia and Africa, where 60% of the world already lives. Migration on that scale means forest land is destroyed to create residential areas. Wild animals, forced to move closer to cities and towns, inevitably encounter domestic animals and the human population. Wild animals often harbor viruses; bats, for instance, can carry hundreds of them. Viruses, jumping from species to species, can ultimately infect people. Eventually, extreme urbanization becomes a vicious cycle: more people bring more deforestation, and human expansion and the loss of habitat ultimately kills predators, including those that feed off rodents responsible of zoonotic disease.
On both of these continents (meaning Asia and Africa) many families depend on farming and a minuscule supply of livestock. Disease control, feed supplementation and housing for those animals is extremely limited.

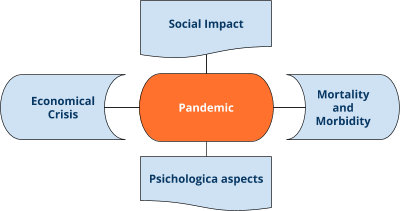
The direct impact of pandemics on health can be catastrophic, in terms of mortality and morbidity; for example, the HIV/AIDS pandemic has killed more than 35 million people since 1981.
Pandemics may lead health systems to collapse and indirect impacts on health can further increase morbidity and mortality rates. Drivers of indirect impact on health include diversion or depletion of resources used to provide routine care and decreased access to routine care, resulting in further deaths. Pandemics constitute a catastrophe not only in terms of public health but also economic and social wellbeing. The health measures implemented to contain the pandemic, including a complete lockdown, suspending work-related activities, travel and trade, lead to a global crisis with long term repercussions.
A pandemic also has a significant psychological impact because it arouses fear and feelings of panic and uncertainty, as well as causing people who catch the disease or come from the contaminated zones to be stigmatized.
Pandemics can cause acute, but also longer-term damage to economic growth. Negative economic growth shocks are directly driven by labor force reductions caused by sickness and mortality, and indirectly by fear-induced behavioral changes. Fear manifests through multiple behavioral changes. The reduction in demand caused by aversive behavior (such as the avoidance of travel, restaurants, and public spaces, as well as workplace absenteeism) exceeds the economic impact of direct morbidity and mortality-associated absenteeism.
During a severe pandemic, all sectors of the economy—agriculture, manufacturing, services—face disruption, potentially leading to shortages, rapid price increases for staple goods, and economic stress for private firms and governments.
Evidence suggests that epidemics and pandemics can have significant social and political consequences, creating clashes between states and citizens, eroding state capacity, driving population displacement, and heightening social tension and discrimination, particularly in fragile states with legacies of violence and weak institutions.
Large-scale outbreaks of infectious disease have direct and consequential social impact. For example, widespread public panic during disease outbreaks can lead to rapid population migration. Finally, outbreaks of infectious disease can cause already vulnerable social groups, such as ethnic minority populations, to be stigmatized and blamed for the disease and its consequences.
Pandemics arise when the infective agent escapes the control measures set up by the health authorities to contain it, leading to collapse of the healthcare system. The sudden influx of large numbers of sick individuals to health facilities stretches the systems’ capacity and resources, even more so and more noticeably where resources are already scarce. When an epidemic emerges and spreads, it inevitably draws most of health responders’ attention and monopolizes most of the health system’s human and financial resources, as well as medical products and technologies. People, efforts, and medical supplies all shift to respond to the emergency. This often leads to the neglect of basic and regular essential health services. People with health problems unrelated to the epidemic find it harder to get access to health care services. Some may die as a result, if the disruption overwhelms the health system. Mortality rates of other diseases for which people could not get treatment may rise. Furthermore, health care settings, and especially emergency rooms, can become hubs of transmission. Many people get infected there, if prevention and control measures are not properly implemented.
Because health care environments and emergency rooms are usually crowded, the lack of appropriate infection prevention and control, for example through triage, isolation, and other precautions, can be very significant. Health workers at the frontline of the response may themselves become infected and die. In countries where there are health staff shortages, the loss of several more health workers further weaken the health system.

Human behavior plays an important role in the spread of infectious diseases and understanding the influence of behavior on the spread of the disease can be key to improving control efforts. Human behavior is based on attitudes, belief systems, opinions and awareness of a disease, and all these factors are crucial elements to reduce contagion.
Communication plays a significant role in the control of an emerging epidemic or pandemic by providing information that people can use to take protective and preventive action. The dissemination of basic information (such as how the pathogen is transmitted, guidance on managing patient care, high-risk practices, and protective behavioral measures) can rapidly and significantly reduce the transmission of disease. The information must be clear, simple, and delivered by official channels: newspapers, TV stations, websites and public health authorities. For example, decisions about vaccines can be influenced by opinions and beliefs that can spread much faster than the corresponding disease. The vaccination policies of a large number of countries are based on voluntary compliance and the drop in vaccination coverage has led to the re-emergence of certain preventable diseases.
However, a multitude of behavioral changes can reduce the spread of infectious diseases, such as the reduction in the number of potentially infectious contacts, wearing face masks or practicing better hygiene. Proper information and awareness of a spreading disease can influence protective behavioral changes, such as respect for quarantine measures, reducing traveling, seeking treatment earlier etc.

Planning and preparing for pandemics are tasks that should be carried out by national governments and international organizations. The WHO writes recommendations and guidelines, although there is no organized system implemented worldwide to review how prepared the different countries are for epidemics, or to measure their rapid response abilities.
The COVID-19 pandemic revealed that several wealthy nations healthcare systems were not prepared and were completely overwhelmed, due to lack of equipment for intensive care, beds and other medical needs. Indeed, shortages were expected to occur even earlier on in the pandemic. The World Health Organization (WHO) and the World Bank warned about the risk of pandemics throughout the 2000s and 2010s, especially after the 2002–2004 SARS outbreak. In 2018, the WHO coined the term, Disease X, which “represents the knowledge that a serious international epidemic could be caused by a pathogen currently unknown to cause human disease” in order to focus research and development on likely candidates for the next unknown pandemic. International divisions and a lack of suitable collaboration limits preparedness.
A number of organizations have been involved for years in preparing the world for epidemics and pandemics, trying to produce a platform for dealing with emerging epidemic disease such as COVID-19, which would enable rapid vaccine development and immunity research in response to outbreaks. Since several centuries, scientists have become increasingly better at interpreting many aspects of the world, including the orbit of planets, the ebb and flow of tides and the paths of hurricanes. The ability to understand natural and physical systems well enough to make accurate forecasts is perhaps one of humanity’s greatest achievements.
There are limits, however, in predicting when the next disease outbreak will happen, because the most important variables can change significantly from one outbreak to another.
Infectious disease is caused by a transmissible pathogen. The infectiousness of that disease can be summarized in a number called the “basic reproductive ratio,” or R0, a number describing how widely a pathogen is likely to spread in a given population.
If epidemiologists know enough about a pathogen’s R0, it is hoped that they can predict aspects of its next outbreak – and possibly prevent small-scale outbreaks from becoming large-scale epidemics. They could achieve this by mobilizing resources to areas where pathogens have especially high R0 values or by limiting interactions between the carriers of disease and the most susceptible members of a given society, often children and the elderly.
The features of an epidemic – the pathogen’s contagiousness, rate of transmission, the availability of vaccines and so on, change rapidly during the course of a single outbreak. Epidemics are often not precise phenomena but complex scenarios where many variables play essential but shifting roles. There is no underlying truth about a disease – only an unstable collection of details that vary, often becoming entangled, as the disease spreads.
Disease surveillance remains a high-stakes area of science. Careful consideration for unique circumstances causing outbreaks, and more responsible collection of data, could save countless lives.
Preventive measures are required to prevent pandemics including measures to reduce causes of new infectious diseases and to prevent outbreaks and epidemics from becoming pandemics. An important way to prevent pandemics is to invest in research; i.e., by identifying new pathogens. Some scientists are screening blood samples from wildlife for new viruses. Pathogen detection mechanisms may allow the construction of an early warning system to identify common features and develop countermeasures and vaccines against a whole categories of viruses. An essential measure is to develop quick testing and strategies for the prevention, early recognition and control of infectious diseases. Ensuring the biosafety level of laboratories may also be an important component of pandemic prevention. Strategies to contain chains of transmission may include:
Air traffic:
- establish preventive countermeasures;
- create concrete recommendations for actions by airport operators and airline companies;
- develop technology to screen people at airport security points, thermometers and medical guidance apps to plot and map unusual fever levels.
In addition, accelerating the creation of new vaccines, drugs and diagnostic tools for global health.

Mitigation is necessary to keep mortality as low as possible and it also keeps effects on the economy within manageable levels. Mitigation countermeasures include:
- mandatory quarantine;
- preventing mass gatherings;
- closure of educational institutes or places of work where infection has been identified;
- isolation of households, towns, or cities.
These measures prevent transmission from symptomatic and non-symptomatic cases, hence flattening the epidemic and pushing the peak further into the future. Social distancing provides time for the health services to treat cases and increase their response capacity, and in the longer term, for vaccines and treatments to be developed. Individual action is also crucial to control the spread of an infection. Personal, rather than government action, in western democracies might be the most important issue; early self-isolation, seeking medical advice remotely unless symptoms are severe, and social distancing are key actions. Government actions to ban mass gatherings are important, and government communication strategies to keep the public informed of how best to avoid infection are vital.
Rapid actions by national and international health authorities are necessary to slow transmission and break the chain of transmission, before an epidemic may become a pandemic.
Detection, investigation, and reporting of the first cases must happen quickly for rapid containment of a pandemic to be possible. Ultimately, the decision to launch a containment operation lies with national authorities. The basic containment strategy uses a geographically based approach in which antiviral medications and non-pharmaceutical measures are used within a defined area surrounding the initial cases to restrict the virus from spreading beyond the Containment Zone. WHO protocols should be used by countries as a foundation to build more detailed operational plans and procedures, as well as by international groups that may have a substantial role in these operations. They will be updated and revised as new information becomes available and more detailed guidance and tools are developed. Countries are strongly encouraged to develop and integrate containment planning into their national pandemic influenza preparedness plans.

Pandemics pose particular challenges when attempting to draw up a visual representation with graphs, bars and charts. One of the most common forms of visualization of the trend over time of a disease in a population is represented by a graph, in which the number of new cases (incidence) is placed in the vertical axis and the time in the horizontal axis. The graph obtained from the data collected during an epidemic generates an “epidemic curve” (more correctly represented by a bar chart). The epidemic curve provides valuable insights into the course of an epidemic, and can help answer important questions such as: what was the path of spread of the disease? when did exposure to the disease agent occur? what was the incubation period? Were there any secondary cases? The course of the disease over time, reproduced by the bars or by the shape of the curve, can also be useful for developing hypotheses about the cause of the disease and its epidemiological characteristics as well as for making predictions about its future course.
While epidemic curves are used to represent a disease as a function of time, there are cases in which it is useful to illustrate the geographical (or spatial) distribution of the disease.
During past epidemics, authorities and responders looked to maps for updated details about confirmed cases, highest risk populations, and available or needed health-care resources.
Disease surveillance is now a map-centric activity, with geographic information system (GIS) technology being used to collect, analyse, and share key data.
In the simplest case, the spatial distribution is summarized in a map which shows the frequency of existing cases at a given instant (prevalence map) or the new cases that have appeared in a given period of time (incidence map).

Selected References
- Managing epidemics key facts about major deadly diseases. WHO,SBN 978-92-4-156553-0
- WHO. “SARS: How a global epidemic was stopped”(PDF). Retrieved 25 March2020.
- Lu, Michael C. “What the world can do to halt future pandemics”. Newsday. The Washington Post. Retrieved 5 June2020.
- Watts, Charlotte H.; Vallance, Patrick; Whitty, Christopher J. M. (18 February 2020).“Coronavirus: global solutions to prevent a pandemic”.Nature.578 (7795): 363
- Morse, et Al “Prediction and prevention of the next pandemic zoonosis”. The Lancet.380 (9857): 1956–1965.:
- “To prevent pandemics, bridging the human and animal health divide”. Salon. 1 June 2020. Retrieved 8 June2020.
7.Cheng e Al “Severe Acute Respiratory Syndrome Coronavirus as an Agent of Emerging and Reemerging Infection”. Clinical Microbiology Reviews.20 (4): 660–694.doi:10.1128/CMR.00023-07.
- Kahn, Jennifer (21 April 2020).“How Scientists Could Stop the Next Pandemic Before It Starts”. The New York Times. Retrieved 8 June2020.
Web Resources
WHO, World Health Organization